Clinical Research
Bicon’s research focuses on a design that has remained unchanged since 1985. While other manufacturers claim decades of research, most of this research had been conducted on designs that are no longer on the market today. Please find a selection of publications on the Bicon system below.
![]() Schulte, J., Flores, A., Weed, M., Crown-to-implant ratios of single tooth implant-supported restorations, Journal of Prosthetic Dentistry, Vol 98, Issue 1, July 2007, Pages 1-5
Schulte, J., Flores, A., Weed, M., Crown-to-implant ratios of single tooth implant-supported restorations, Journal of Prosthetic Dentistry, Vol 98, Issue 1, July 2007, Pages 1-5
Background: The crown-root ratio guidelines used to establish a prognosis for teeth serving as abutments are commonly applied to a dental implant-supported restoration or potential implant site. These guidelines are generally empirical and therefore lack scientific validation. The purpose of this study was to first determine the crown-implant ratios of single tooth implant-supported restorations, and then to compare the crown-implant ratios to the guidelines established for the crown-root ratios of natural teeth.
Methods: A retrospective cohort study design was used. The cohort was composed of subjects (n=294) having 1 or more single tooth implants (Bicon) placed between May 1992 and April 2004. A chart review was conducted to obtain radiographs in which the entire crown and implant were visible. The length of the crown and implant were measured directly from the radiographs using magnification to calculate the crown-to-implant ratio. The length of the crown was divided by the length of the implant to determine the crown-implant ratio. Calculations were made to within 0.1 mm. Implant failure was recorded and defined as removal of the implant for any reason. Data were analyzed with descriptive statistics.
Results: A total of 889 single tooth implants from 294 patients were measured and included in the study. The mean (SD) follow-up time was 2.3 (1.7) years, with a range of 0.1 to 7.4 years. Sixteen failures were recorded for a survival rate of 98.2%. The crown-implant ratios ranged from 0.5:1 to 3:1. The mean (SD) crown-implant ratio of implants in function was 1.3:1 (0.34). The mean crown-to-implant ratio of failed implants was 1.4:1 (2.5).
Conclusion: The results of this study suggest that the crown-to-root ratio guidelines associated with natural teeth should not be applied to a potential implant site or existing implant restoration. The crown-to-implant ratios of those implants that were in function were similar to those implants that failed.
![]()
![]() Venuleo, C., Chuang, S.K., Weed, M., Dibart, S., Long term bone level stability on Short Implants: A radiographic follow up study, Indian Journal of Maxillofacial and Oral Surgery September 2008, Vol. 7: No.3, p. 340-345.
Venuleo, C., Chuang, S.K., Weed, M., Dibart, S., Long term bone level stability on Short Implants: A radiographic follow up study, Indian Journal of Maxillofacial and Oral Surgery September 2008, Vol. 7: No.3, p. 340-345.
Background: Placement of short endosseous implants represents a valid tratment alternative to more complex surgical techniques such as ridge augmentation/sinus lift implant-associated procedures, in the setting of limited alveolar bone height. This study’s objectives were: 1) to estimate the 5-year clinical survival of Bicon 6×5.7mm implant 2) to evaluate radiographic bone level changes around 6×5.7mm implants in comparison with Bicon longer non-6×5.7mm implants.
Methods: A retrospective cohort study design was used. The cohort was composed of patients who had at least one 6×5.7mm implant placed for 5 years, at least one non-6×5.7mm implant, and who were willing to return to the dental office for radiographic evaluation. A total of 141 implants, 32 6×5.7mm (test group) and 109 non-6×5.7mm (control group), were placed in 20 patients (12 males and 8 females) with a mean age of 59.2 +/- 11.8 years. Mean length of non-6×5.7mm implants was 9.7 mm, (range: 8 mm to 14 mm, mean diameter was 4.39 mm (range: 3.5 mm to 5 mm). Bone loss, defined as the vertical difference in crestal bone level measurements from the baseline (day of implant placement) to 5 years follow-up, was digitally determined on periapical radiographs. Generalized linear mixed models were used for the statistical analysis.
Results: Five-years survival rates for test and control groups were 90.3 % and 97.7% respectively, but this difference was not statistically significant (p>0.05). There was no significant difference between the two groups with regard to mean changes of radiographic bone levels.
Conclusion: Short implants with large diameter (6×5.7mm) have a long-term (>5 years) survival rate and crestal bone level maintenance similar to that observed for non-6×5.7mm implants. The results of this radiographic study support the hypothesis that 6×5.7mm implants can be successfully used in edentulous maxillary and mandibular areas with limited bone height.
![]()
![]() Gentile, M., Chuang, S.K., & Dodson, T., Survival Estimates and Risk Factors for Failure with 6 x 5.7 mm Implants, The International Journal of Oral & Maxillofacial Implants,
Gentile, M., Chuang, S.K., & Dodson, T., Survival Estimates and Risk Factors for Failure with 6 x 5.7 mm Implants, The International Journal of Oral & Maxillofacial Implants,
Vol. 20, No. 6, p. 930-937, November/December 2005.
Purpose: Short dental implants facilitate prosthetic restoration in the setting of limited alveolar bone height. The study objectives were to (1) estimate the 1-year survival of Bicon 6 x 5.7mm implants, (2) compare the 1-year survival of 6 x 5.7mm implants with that of non–6 x 5.7mm implants, and (3) identify risk factors associated with implant failure.
Materials and Methods: A retrospective cohort study design was used. The sample was composed of patients who had received at least one 6 x 5.7mm implant. Predictor variables were categorized as demographic, health status, anatomic, implant-specific, prosthetic, perioperative, and reconstructive.
The outcome variable was implant failure, defined as explantation. Appropriate descriptive, bivariate, and multivariate survival statistics were computed. results: The sample was composed of 35 patients in whom 172 implants had been placed (45 of which were 6 x 5.7mm). The 1-year survival rates for 6 x 5.7mm and non–6 x 5.7mm implants were 92.2% and 95.2%, respectively (P = .76). After adjusting for covariates in a multivariate model, implant size was not associated with failure
(P = .95).
Discussion: The comparable survival estimates for 6 x 5.7mm implants and non–6 x 5.7mm implants in this study suggested that 6 x 5.7mm implants can become osseointegrated and bear a functional load after placement.
Conclusions: The survival of 6 x 5.7mm implants was comparable to that of non–6 x 5.7mm implants.
![]()
![]() Dibart, S., Warbington, M., Su, M.F., Skobe, Z., In
Dibart, S., Warbington, M., Su, M.F., Skobe, Z., In
Vitro Evaluation of the Implant-Abutment Bacterial Seal: The Locking Taper System, Journal of Oral and Maxillofacial Surgery, Vol. 20, No. 5, p. 732-737, September 2005.
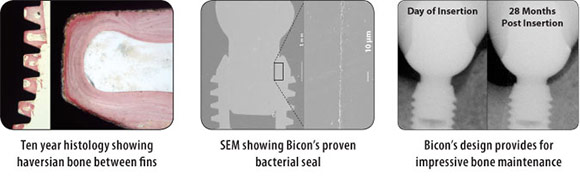
Purpose: To test in vitro whether the seal provided by the locking taper used in the implant-abutment connection was capable of preventing the invasion of oral microorganisms.
Materials and Methods: Twenty-five wide-body implants (5 x 11 mm) and 25 abutments were divided into 2 groups for a 2-phase experiment. The first phase tested the ability of the seal to shield the implant well from outside bacteria; the second phase tested the ability of the seal to prevent bacteria present in the implant well from seeping out. For phase 1, 10 implant-abutment units were immersed in a bacterial broth for 24 hours. The abutments were then separated from the implants and bacterial presence was evaluated using scanning electron microscopy. In phase 2, the tested abutments were inoculated with a droplet of soft agar bacterial gel and assembled with the implant. These units were incubated in a sterile nutrient broth for 72 hours, sampled, and plated to assess bacterial presence. results: In phase 1, no bacteria were detected in any of the implant wells. In phase 2, no bacteria were detected in the nutrient broth or on the agar plates at 72 hours.
Discussion: In implants where a microgap is present, microbial leakage could lead to inflammation and bone loss; thus, it is important to minimize bacterial presence in and around the the implant-abutment junction.
Conclusion: The seal provided by the locking taper design has been demonstrated to be hermetic with regard to bacterial invasion in vitro.
![]()
![]() Bozkaya, D., and Müftü, S., Muftu, A., Evaluation
Bozkaya, D., and Müftü, S., Muftu, A., Evaluation
of Load Transfer Characteristics of Five Different Implant Systems in Compact Bone at Different Load Levels by Finite Element Analysis, Journal of Prosthetic Dentistry, Vol. 92 No.6, p.523-530, December 2004.
Statement of Problem: The external contour of an implant and the magnitude of occlusal loading can have significant effects on the load transfer characteristics and may result in different bone failure rates for different implant systems.
Purpose: The goal of this study was to investigate the effects of external geometry and occlusal load magnitude on bone failure modes for 5 commercially available dental implant systems.
Materials and Methods: Five different implant systems; Ankylos, Astra, Bicon, ITI, and Nobel Biocare, comparable in size, but different in thread profile and crest module shapes, were compared using the finite element method. Type II bone quality was approximated and complete osseous integration
was assumed. Occlusal loads of varying magnitudes (0 to 2000 N) were applied on the abutments supporting single tooth restorations at 11.3 degrees from the vertical axis with a 1-mm offset. Total overloaded bone area, where tensile and compressive normal stresses fell outside of the recommended limits of 100 and 170 MPa, respectively, was investigated for different load levels.
Results: For moderate levels of occlusal loads up to 300 N, the compact bone was not overloaded by any of the implant systems. At the extreme end of the occlusal load range (1000 N or more) the overloading characteristics of implants may be dependent on geometric shape.
Conclusion: In general, overloading occurs near the superior region of compact bone, in compression, and it is primarily caused by the normal and lateral components of the occlusal load. At the region of intersection of compact and trabecular bone, overloading occurs in tension due to the vertical
component of the occlusal load. For excessive forces greater than 1000 N, the overloaded areas of the bone varied considerably among 5 different implants systems evaluated.
![]()
![]() McDermott, N., Chuang, S.K., Vehemente, V., Dodson, T.B., Complications of Dental Implants: Identification Frequency and Associated Risk Factors, The International Journal of Oral & Maxillofacial Implants, Vol. 18, No.
McDermott, N., Chuang, S.K., Vehemente, V., Dodson, T.B., Complications of Dental Implants: Identification Frequency and Associated Risk Factors, The International Journal of Oral & Maxillofacial Implants, Vol. 18, No.
6, p. 1379-1389, December 2003.
Purpose: This study sought to identify the types, frequencies, and risk factors associated with complications following placement of dental implants. It was hypothesized that one or more factors could be identified that are associated with an increased risk for complications and may be modified by the clinician to enhance outcome.
Materials and Methods: A retrospective cohort study design was used that included patients who received Bicon implants (Bicon, Boston, MA) between 1992 and 2000. Predictor variables were grouped into demographic, medical history, implant-specific, anatomic, prosthetic, and reconstructive categories. Complications were grouped into inflammatory, prosthetic, operative, and major or minor categories. Cox proportional hazards regression models were developed to identify risk factors for complications.
Results: The sample was composed of 677 patients. The overall frequency of implant complications was 13.9% (10.2% inflammatory, 2.7% prosthetic, 1.0% operative), of which 53% were minor. The multivariate Cox model revealed that smoking, use of 1-stage implants, and reconstructive procedures were statistically associated with an increased risk for overall complications (P < or = .05). The median duration of follow-up was 13.1 months (range 0 to 85.6 months).
Discussion: A lower frequency of complications was found compared to mean frequencies calculated from past reports. Investigations examining the influence of smoking and reconstructive procedures on implant complications are recommended.
Conclusion: Of the 3 factors associated with an increased risk for complications, tobacco use and implant staging may be modified by the clinician to enhance outcome.
![]()
![]() Keating, K., Dublin Institute of Technology, Department of Engineering Technology, Connecting Abutments to Dental Implants ‘An Engineer’s Perspective’, Irish Dentist, July 2001.
Keating, K., Dublin Institute of Technology, Department of Engineering Technology, Connecting Abutments to Dental Implants ‘An Engineer’s Perspective’, Irish Dentist, July 2001.
Osseointegrated implants are one of the fastest growing dental treatments in Ireland today. They are not new, implant restorations have been in use for over 30 years now. They are used singularly as replacement for single tooth loss and as the support for a bridge either to a natural tooth or to another implant.
Multiple implants are also used to support prostheses, e.g. full or partial dentures.
An implant is a mechanical system designed to transmit occlusal forces on a prosthesis through an abutment and implant to the surrounding bone. In the United States alone, there are more than 50 companies involved in manufacture or marketing of dental implants. Brunski (1999) states that implant design is driven by
copying and modifying existing designs rather than fundamental advances in biomechanics.
The original and most copied method of attaching the abutment to the implant is by means of a screw. It is still the method common to most implant systems. Screw loosening and screw breakage is a major disadvantage of this method. Jemt et al (1991) have shown that screw loosening appears to be a bigger problem with single tooth restorations.
There is an alternative to screw retained abutment systems; a Boston based implant company called Bicon uses a locking taper system to connect the abutment. In this article, I will give an engineers perspective on these two methods of connecting the abutment to the implant.
![]()
For a more comprehensive list of publications, please use the following link: